Olivia's Story
Jenna Beck
The following story has been provided to us by Oliva's family and has been included exactly as received.




July 29th 2008 our little surprise package arrived.
After a speedy delivery Olivia was taken to the special care nursery (SCN) at Hurstville Community Private Hospital where she was struggling to take each breath. We could see her little chest being sucked in as she tried to breathe. I remember thinking that it was probably just that she had been born so quickly. After the pediatrician examined her he diagnosed her with Pierre Robin Sequence.
We then went down to the SCN to look at our daughter through 'new' eyes. I felt totally dazed and in shock and I didn’t even realise what was ahead of us at that point. I just wanted to hold her. That feeling of shock and surrealism lasted well into Olivia’s 1st month and probably until we got her home. That is when we got a good dose of reality! A baby on CPAP, my other daughter on the brink of terrible twos, me expressing breast milk and my husband madly trying to keep afloat operating his business!!!!!
So back to Olivia. After a week at Hurstville she was transferred by intensive care ambulance to the Royal Womens Hospital at Randwick. She spent 2 weeks there in Neonatal Intensive Care where she learnt to suck from a bottle using a Chu Chu teat designed for children with Cleft conditions. We started to discover what a little personality she was at this stage when she took her own nasogastric feeding tube out and never looked back! Whilst there we also had to endure 2 sleep studies where it was discovered she had obstructive sleep apnea and would need to come home using a cpap machine and an apnea monitor which would alarm should she stop breathing for more than 20 seconds. She had numerous tests including a full body X- Ray to rule out various other syndromes that can be linked to PRS. We learned that her heart, lungs, eyes, ears and bones were all fine. She has no genetic or chromosomal abnormalities, so thankfully it appears to be an isolated case of PRS. Our life whilst Olivia was at RHW consisted of dropping Charlotte at my mums in the morning, driving to Randwick, doing whatever I could for Olivia, expressing, stressing then driving back to mums to get Charlotte spend time with her, put her to bed, then when Craig , my husband go home I would go back to the hospital, practice feeding Olivia, express, sit there and look at her, try to make sense of what had been written on her chart and then drive home. A very stressful time for all of us!
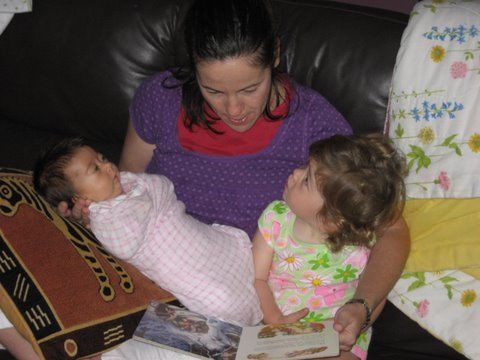
At 2 months old Olivia finally came home and didn’t she love it! She was so happy and seemed to really love being wrapped up and put into her cot! After being in hospital for all those weeks you can imagine her wide eyes at seeing all the colour and noises of the outside world! Charlotte finally began to understand what having a baby sister meant.
I found it amazing how Charlotte accepted the CPAP as part of Olivia’s sleep routine and she would often help by carrying the apnea monitor or remind us if we forgot to attach it!
I guess Craig and I realized what it meant to have two children under two rather than one! Once we had Olivia home the medical issues seemed less significant as we saw her doing all the ‘normal’ baby things. But here began our battle with the CPAP. Slowly, slowly each week Olivia would seem to tolerate the CPAP less and less. After another sleep study we were excited to discover she had gone from 61 obstructions per hour whilst asleep to 17!!! So we reduced the pressure but again she started to reject it. Finally at 4 months we had a 4th sleep study and she slept the whole night safely! No more CPAP! It was the best Christmas present we could ever hope for.
Come May 18th 2009 she will have her palate repaired, there is a slim chance that this will start her breathing problems again but we are trying not to think about that!
We have been lucky and as I write this I believe it. We have had wonderful support from family and friends. There will still be many hurdles to jump and tears to shed but forever we have a beautiful, happy little girl to love and cherish.
At 10 months Olivia had her palate repaired. It was more stressful for me than Olivia. She recovered so quickly it was amazing. Due to her previous breathing problems they left the naso phararyngyl tube in as a precaution. Olivia hated this and after two days they took it out and she began eating and drinking again and never looked back. The arm restraints( to stop Olivia from putting her hands and sharp objects in her mouth) which I was dreading, turned out to be a blessing at the park. They did not stop Olivia from playing, crawling, pulling up but they did stop her from eating bark chips, sand, rocks- a few of her favorites at the park. She can now suck from a straw, is enjoying her finger foods, she is a robust healthy little 1 year old.
At her 12 month check ups with the GP, Plastic surgeon, audiologist, ENT surgeon and speech therapist I was so happy to find that her height, weight are all average. Her ears are perfect- she passed her hearing test with flying colours, her speech- well babble, screeching and communication skills are right on target and her palate looks great. That slim chance of breathing problems occurring post op… Well she is again affected by OSA (Obstructive sleep apnoea) 11.9 obstructions per hour, the longest was 16 seconds, however we are treating this with steroidal nasal spray for now. There will be more sleep studies in the future ( every six months unless there are any concerns before) but we are all so happy to not be dealing with the CPAP again.
A friend asked me the other day.. 'Of all the professionals you are dealing with whose advice have you found the best.' After thinking about it I realized we have been lucky to be dealing with so many caring people but most of all our GP is an absolute gem. He is always on hand to give advice, point us in the right direction or calm me down when someone else has said something to offend or upset. I really believe it is so rare these days to find a GP that actually cares and will go above and beyond the call of duty to help a patient. Having said that our paediatrician was fabulous right there in the beginning- he even gave me his mobile phone number so I could call him anytime. He made special trips to the hospital to see us and often after he had done the rounds with the big wigs he would come back and whisper ‘did you understand all that?’ The other great person that deserves to be remembered and mentioned in Olivias story is Melissa Parkin. A great speech therapist at Sydney Kids who deals with feeding problems in babies. With Melissa I had my first positive experience with Olivia. It makes me cry to write that and to think that it was a good two weeks before I actually had a positive experience with Olivia and thought I can look after this baby and she will get better and things can go forward. With her assistance Olivia learned to get that precious milk from the bottle. She was always so positive and encouraging and it was her persistence that put Olivia on the road to being so healthy and robust as she is today. We were able to come home tube free as Olivia was taking full feeds from a regular bottle using the Chu Chu teat. Once home, however, she failed to 'thrive' as her calories were being used up in the extra efforts to breathe. We were able to combat this with one scoop of formula per 24 hours added to her milk.
There are just no words to thank these people for what they have done for us. All I can hope is that good and positive things will come their way.
